Let's be honest, if you're dealing with chronic constipation, you know it’s so much more than a little discomfort. It's a frustrating, persistent problem that can completely throw off your day, leaving you feeling bloated, uncomfortable, and just plain stuck. This isn't about missing a bowel movement for a day or two—it's a recurring battle …
Let's be honest, if you're dealing with chronic constipation, you know it’s so much more than a little discomfort. It's a frustrating, persistent problem that can completely throw off your day, leaving you feeling bloated, uncomfortable, and just plain stuck. This isn't about missing a bowel movement for a day or two—it's a recurring battle that takes a real toll, both physically and emotionally.
To find real relief, we have to move beyond a simple definition. Sure, chronic constipation is often defined as having fewer than three bowel movements a week, but the actual experience is so much bigger than that number.
Recognizing the Symptoms
The signs of chronic constipation paint a much clearer picture of what's really going on. It’s rarely just about frequency. Many people I work with struggle with a combination of these issues:
- Straining During Bowel Movements: That feeling like you have to put in a serious effort just to pass stool.
- Hard or Lumpy Stools: When what finally comes out is hard, dry, and pellet-like, making it difficult to pass.
- A Sense of Incomplete Evacuation: The nagging feeling that you haven't fully emptied your bowels, even after you've gone.
- Feeling of Blockage: A very real sensation that something is physically blocking the stool from passing.
- Abdominal Bloating and Pain: Persistent gas, cramping, and a swollen belly just add to the misery.
These physical symptoms can easily spiral into a cycle of anxiety and stress around going to the bathroom, which, ironically, can make the constipation even worse. It’s so important to understand that this is a legitimate medical issue, not just a minor inconvenience. Acknowledging that is the first step toward empowering yourself to find solutions that actually work.
You Are Not Alone in This Struggle
It’s easy to feel isolated when dealing with digestive problems, but chronic constipation is incredibly common. In the United States alone, it's estimated that chronic idiopathic constipation (CIC) affects 9% to 20% of adults.
That's millions of people. This isn't just a personal problem; it's a massive public health issue, leading to around 2.8 million medical visits for constipation in a single year. It's especially common among older adults—up to 40% of people over 65 report it as a regular struggle. You can read the full research about constipation's impact on public health to see just how widespread this is.
This isn't just a personal discomfort; it's a widespread health concern with real consequences. Recognizing its prevalence can be the first step in demystifying the condition and taking proactive steps toward management.
When you grasp the true scope of the problem, you can shift your perspective. This isn't a personal failure—it's a manageable health condition that millions of others share. By understanding what chronic constipation is, recognizing its many symptoms, and knowing you’re not alone, you can start building a solid foundation for finding lasting relief and getting back to feeling like yourself.
Building a Pro-Motility Diet
If you've ever been told to just "eat more fiber" to relieve chronic constipation, you know how frustrating and simplistic that advice can feel. While it’s well-intentioned, it completely misses a critical detail: not all fiber is created equal.
Building a diet that actually encourages healthy gut motility is less about following some rigid plan and more about understanding how specific foods can work with your body. It’s about making smart, sustainable choices that help your digestive system get back on track, without causing more bloating or discomfort.
The Two Faces of Fiber
The secret to making fiber work for you lies in understanding its two main forms: soluble and insoluble. Think of them as a team working together to keep things moving. Getting the right balance is the key to finally finding relief.
-
Soluble Fiber: This type dissolves in water, creating a gel-like substance in your digestive tract. Its main job is to soften your stool, making it much easier to pass. You'll find it in foods like oats, barley, nuts, seeds, beans, lentils, and fruits like apples and citrus.
-
Insoluble Fiber: This type doesn't dissolve. Instead, it adds bulk to your stool, which helps stimulate the intestines and speeds everything along. You can get it from whole grains, the skins of fruits and vegetables, and nuts.
For many people I see who are struggling with constipation, focusing on increasing soluble fiber first is often the most effective strategy. It gently softens things up without the sometimes-harsh bulking effect of too much insoluble fiber, which can occasionally make matters worse if you're already backed up.
Strategic Foods to Add to Your Diet
You don’t need to overhaul your entire life overnight. Just incorporating a few specific, high-impact foods into your meals can make a huge difference. The goal is consistency, not perfection.
Chia Seeds and Flaxseeds
These tiny seeds are absolute powerhouses of soluble fiber. Just a single tablespoon of chia seeds packs about 5 grams of it. They're incredibly easy to add to oatmeal, yogurt, or smoothies. My favorite trick? Create a simple chia seed pudding by mixing them with a plant-based milk and letting it sit in the fridge overnight.
Kiwis and Prunes
These fruits are famous remedies for a reason—they work. Studies have actually shown that eating two kiwis a day can significantly improve bowel function in people with chronic constipation. Prunes (or dried plums) are another classic, containing both fiber and sorbitol, a natural sugar alcohol that acts as a gentle osmotic laxative by drawing water into the colon.
A small study suggested that eating around 100 grams of prunes (about 10 prunes) daily was more effective at improving stool frequency and consistency than psyllium husk, a common fiber supplement.
Legumes
Beans, lentils, and chickpeas are fantastic sources of both soluble and insoluble fiber. If you're not used to eating them, the key is to introduce them slowly to avoid gas and bloating. Start by adding just a quarter-cup to a salad or soup a few times a week, and then gradually increase the amount as your system gets used to it.
Here’s a quick guide to help you get more of these helpful fibers into your diet.
Your Guide to High-Fiber Foods
This table offers a practical list of foods rich in both soluble and insoluble fiber. Use it as a handy reference when you're planning meals to support better digestive flow.
| Food Source | Type of Fiber | Serving Size | Approx. Fiber Content (grams) |
|---|---|---|---|
| Chia Seeds | Soluble | 2 tablespoons | 10g |
| Black Beans | Both | 1 cup, cooked | 15g |
| Avocado | Both | 1/2 medium | 7g |
| Oats | Soluble | 1 cup, cooked | 4g |
| Raspberries | Both | 1 cup | 8g |
| Broccoli | Both | 1 cup, chopped | 5g |
| Prunes | Both | 1/2 cup (about 8 prunes) | 6g |
| Lentils | Both | 1 cup, cooked | 16g |
Remember, variety is key. Mixing different sources of fiber will give your gut the diverse nutrients it needs to thrive and keep things moving smoothly.
This infographic gives you a great visual of how to build a plate that naturally supports regularity.
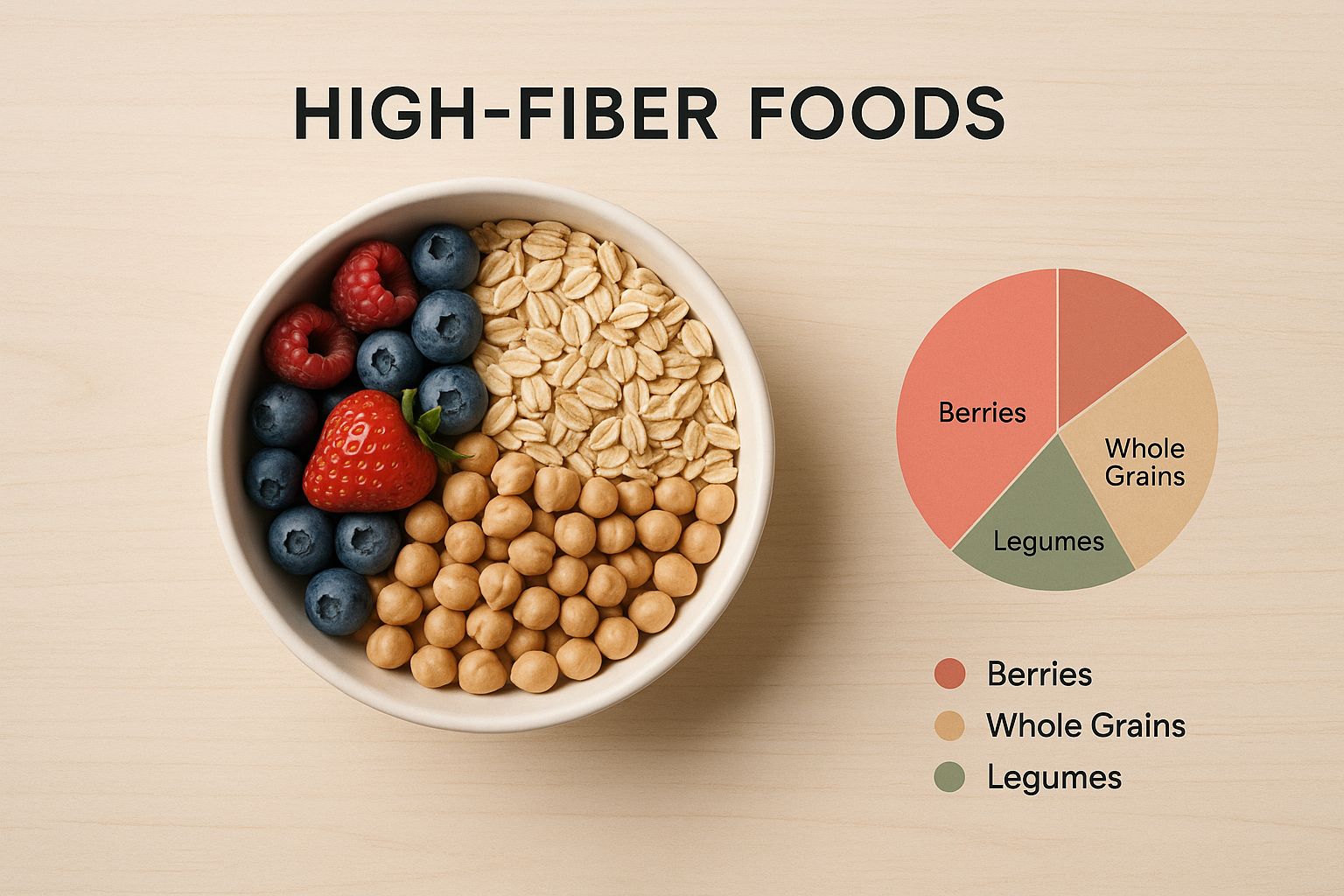
It’s all about creating a balanced mix of colorful fruits, vegetables, grains, and legumes.
The Non-Negotiable Role of Hydration
Here's the deal: you can eat all the fiber in the world, but without enough water, it can't do its job. In fact, loading up on fiber without increasing your fluids can make constipation so much worse.
Water is what allows that soluble fiber to form its beneficial gel, softening your stool so it can pass easily. Think of fiber and water as essential partners. You need both.
Aim for at least 8 glasses (64 ounces) of water per day. You might need even more depending on your activity level, the climate you live in, and how much fiber you're eating.
If plain water feels like a chore, mix it up:
- Try herbal teas like peppermint or ginger.
- Infuse your water with lemon, cucumber, or berries.
- Clear broths and soups also count toward your daily fluid intake.
Think of it this way: fiber is the sponge, but water is what makes it soft and pliable. Without enough water, you're just adding a dry, hard sponge to your system—and that only adds to the blockage. True relief comes from the powerful combination of the right kinds of fiber and consistent, adequate hydration.
Using Movement and Routine to Your Advantage

Lasting relief from chronic constipation isn't just about what's on your plate. Your daily habits—how you move, when you rest, and even how you handle stress—play a massive role in your digestive rhythm. Creating a supportive lifestyle doesn't mean you have to overhaul everything overnight. Instead, it’s about making small, consistent adjustments that tell your body it's safe to let go.
Think of your digestive tract as a long, muscular tube. Just like any other muscle, it works better with regular movement. When you're sedentary for too long, your gut can become sluggish, too. Gentle physical activity is one of the best ways to stimulate peristalsis, those wave-like muscle contractions that push stool through your intestines.
You don't need to start training for a marathon. In fact, for some people, overly intense exercise can make digestive issues worse. The real goal is consistent, moderate movement that encourages regularity.
Gentle Movement for a Healthier Gut
The trick is to find an activity you actually enjoy so you'll stick with it. Just 20-30 minutes of gentle exercise most days of the week can make a huge difference in your bowel habits and how you feel overall.
Consider adding one of these to your daily life:
- A Brisk Daily Walk: This is one of the easiest and most effective ways to get things moving. A simple walk after a meal can really help digestion and stimulate your colon.
- Yoga: So many yoga poses are designed to gently massage your abdominal organs. Twisting poses, in particular, are fantastic for compressing and releasing the colon, which can encourage movement.
- Stretching: Simple stretches that focus on the abdomen and lower back can relieve that tight, bloated feeling, making bowel movements more comfortable.
- Swimming: This is a wonderful low-impact activity that engages your core muscles without putting any stress on your joints.
Remember, the aim is to shorten your intestinal transit time—how long it takes for food to travel through your system. Regular, gentle activity is a powerful tool for this.
The Power of a Consistent Bathroom Routine
Your body absolutely loves predictability. Just like you get sleepy around the same time each night, you can train your digestive system to have a regular rhythm. We often call this bowel training, and it's a surprisingly simple but effective strategy for managing chronic constipation.
It’s all about setting aside a specific time each day to sit on the toilet for about 10-15 minutes, distraction-free. The best time is usually 20-30 minutes after a meal, since eating naturally stimulates the colon—this is called the gastrocolic reflex.
Here’s how to build a routine that works:
- Pick a Consistent Time: For most people, after breakfast is perfect. Your body is rested, and that first meal provides a natural trigger.
- Create a Calm Space: Put your phone away. Don't strain or try to force anything. The whole point is to relax and let your body do its thing.
- Use a Footstool: Propping your feet up with a small stool actually changes your posture, straightening the rectum and making it easier for stool to pass without effort. It mimics a natural squat, which is the ideal position for elimination.
- Be Patient: This can take a few weeks for your body to adjust. Don't get discouraged if nothing happens every time. It’s the consistency that builds the new habit.
This isn't about forcing a bowel movement. It’s about creating a dedicated, stress-free window of opportunity for your body to respond to its natural signals. Over time, this consistency can re-establish a predictable pattern.
Calming Your Gut by Calming Your Mind
The link between your brain and your digestive system is powerful. Ever feel "butterflies" in your stomach when you're nervous? That's the gut-brain axis in action. Chronic stress and anxiety can directly slow down your gut motility, making constipation worse.
When you're constantly stressed, your body is stuck in "fight or flight" mode, which diverts energy away from crucial "rest and digest" functions. Learning to manage stress isn't just good for your mind—it's absolutely essential for your digestive health. For more insights on how holistic approaches can support your well-being, explore the additional resources on our Healing Waters Wellness blog.
Here are a few actionable ways to calm your nervous system and, in turn, your gut:
- Deep Breathing Exercises: Simple belly breathing can activate the vagus nerve, which helps shift your body out of stress mode. Try inhaling slowly for a count of four, holding for four, and exhaling for six.
- Mindfulness Meditation: Even just five minutes of mindfulness a day can significantly lower stress levels. Focus on your breath and just observe your thoughts without judgment. Studies show this practice can really improve digestive symptoms.
- Prioritize Sleep: Not getting enough quality sleep throws your hormones out of whack and increases stress, both of which can aggravate constipation. Aim for 7-9 hours of restful sleep each night.
By combining gentle movement, a predictable routine, and stress management, you create a powerful synergy. You're not just treating a symptom; you're supporting your body's natural ability to function as it should, paving the way for lasting relief.
The Role of Mineral Waters in Gut Health

When diet and exercise aren't quite cutting it, some of the most effective remedies are the ones that have been around for centuries. One of my favorites is balneotherapy—the therapeutic use of mineral-rich waters. This isn't just about drinking more water; it's about using specific "healing waters" to gently get things moving again.
Sourced from natural springs, these waters are packed with minerals like magnesium sulfate and sodium sulfate. These compounds are natural osmotic agents, which is a scientific way of saying they help your colon pull in and hold onto more water. This is the key to softening hard, dry stool, making it much easier to pass.
How Mineral Waters Are Different From Tap Water
Staying hydrated with regular tap water is absolutely essential, but therapeutic mineral waters offer something extra for chronic constipation. While tap water keeps your whole body hydrated, it just doesn't have the high concentration of minerals needed to create that osmotic effect in the colon.
Think of it like this: plain water is for maintenance. It keeps your system running smoothly and helps prevent constipation from starting. Mineral water, on the other hand, is a targeted tool. It delivers specific compounds right where they're needed to actively resolve a backup.
It's no surprise that people are looking for natural solutions. The constipation treatment market is huge—North America once held a 37.8% share, generating billions. This demand is fueled by aging populations and modern lifestyle habits, like not getting enough fiber. You can read more about trends in the constipation treatment market to see just how common this issue is.
How to Safely Use Mineral Waters
If you want to give this a try, the most important things are choosing the right water and starting slow. Don't just grab any bottled water off the shelf. You need to look for one specifically labeled as having a high mineral content, especially magnesium.
Here are a few tips to get you started:
- Start Small: Begin with just one small glass (about 4-6 ounces) a day and see how your body feels. You can always increase it from there if you need to.
- Time It Right: Lots of people find it most effective to drink it on an empty stomach, like first thing in the morning before breakfast.
- Read the Label: Check for the Total Dissolved Solids (TDS). A higher number means more minerals. Specifically, look at the amounts of magnesium (Mg) and sulfate (SO4).
The goal isn't to replace your regular water intake but to supplement it. Use mineral water as a specific tool for those times when you need extra help getting things moving, rather than your primary source of hydration.
This isn't a new fad. European spa cultures have used this method for its digestive benefits for hundreds of years. We're just now understanding the science behind why this traditional practice works so well.
When Is This a Good Approach?
Mineral water can be a game-changer if you’ve already tried increasing your fiber and water intake but still aren't getting consistent relief. It offers a gentle, non-stimulant alternative to some of the harsher over-the-counter laxatives.
Of course, it’s always smart to be cautious with any new remedy. If you have kidney problems or other health conditions, it's a good idea to chat with your doctor before making mineral water a regular thing. For most people, though, it’s a safe and effective way to add another natural strategy to their gut-health toolkit.
Navigating Supplements and Medical Support
So, you’ve been doing everything right. You've cleaned up your diet, you're moving your body more, and you're chugging water like it's your job. But you're still stuck. When lifestyle changes just aren’t cutting it, it might be time to look at other kinds of support. This is where supplements, over-the-counter aids, and a doctor's guidance come in, but it’s so important to approach them the right way to find relief without causing a whole new set of problems.
You're definitely not alone in this. The market for constipation treatments is huge—it was valued at around $12.58 billion just a few years back and is expected to jump to nearly $22.93 billion. That massive number tells you just how many people are looking for the same answers you are. Most of that growth comes from laxatives, simply because they're easy to find. Seeing that landscape, as detailed on transparencymarketresearch.com, can be a little reassuring; this is a common struggle.
Understanding Over-the-Counter Options
Walking down the laxative aisle at the pharmacy can feel overwhelming. Every box promises fast, gentle relief, but they are absolutely not all created equal. Picking the wrong one can easily make your situation worse in the long run.
Here’s a quick rundown of what you’ll find:
-
Bulk-Forming Laxatives: Think of these as fiber in a bottle. Products with psyllium (Metamucil) or methylcellulose (Citrucel) work by absorbing water in your gut, which adds bulk and softness to your stool. This bulk helps trigger a natural muscle contraction to get things moving. They're generally the gentlest choice and safe for longer-term use, but you must drink plenty of water with them or they can backfire.
-
Osmotic Laxatives: These work a bit differently. They pull water from the surrounding tissues directly into your bowels. This extra hydration softens everything up, making it much easier to pass. Common ones you'll see are polyethylene glycol (Miralax) and magnesium hydroxide (Milk of Magnesia).
-
Stimulant Laxatives: These are the heavy hitters. Products with bisacodyl (Dulcolax) or senna (Senokot) work by directly stimulating the nerves in your colon to contract forcefully. They work fast, but they come with a major catch: they should only be used for short-term, emergency situations. If you rely on them, your bowels can become dependent and forget how to work on their own.
When to Seek Professional Medical Advice
Trying things on your own is fine for an occasional backup, but chronic constipation is a different beast. If you find yourself reaching for a laxative more than once or twice a week, that’s your body sending a clear signal that it’s time to call in a professional. A doctor can help you dig deeper to find underlying causes that no amount of fiber or water will fix.
It's crucial to stop self-treating and see a doctor if you experience any red-flag symptoms. These are signs that something more serious could be happening and require immediate medical evaluation.
Be on high alert for these warning signs:
- Severe or persistent abdominal pain that doesn't let up.
- Unexplained weight loss, especially if you aren't trying to lose weight.
- Blood in your stool (this can look like bright red streaks or dark, tarry stools).
- A sudden, dramatic change in your bowel habits that lasts more than a couple of days.
- Anemia (low iron) that shows up on a blood test.
A doctor can investigate these symptoms and rule out things like irritable bowel syndrome (IBS), thyroid problems, or even structural issues within your colon. They also have access to prescription medications like lubiprostone or linaclotide that work in more targeted ways.
If you’re open to exploring complementary therapies, a healthcare professional can also discuss options like colon hydrotherapy, which can provide significant relief for many by gently cleansing and hydrating the colon.
Common Questions on Finding Constipation Relief
Even with a solid plan, it's natural for questions to pop up. Tackling chronic constipation isn't always a straight line—it involves a bit of trial and error. Knowing what to expect can make the whole journey feel a lot less overwhelming. Let's clear up some of the most common questions we hear from people working to find lasting relief.
How Long Until Diet Changes Actually Work?
This is the big one, and the honest answer is: it really depends on your body. Some people start to notice a positive change within just a few days of upping their fiber and water. For others, it might take a good two or even three weeks for their digestive system to adapt to the new normal.
The real keys here are patience and consistency. A classic mistake is adding a ton of fiber all at once, which can totally backfire and leave you feeling even more gassy and bloated. Think of it as a gradual ramp-up, not a flip of a switch. Your body needs time to learn how to process all that good fiber efficiently.
Can I Get Dependent on Laxatives or Mineral Waters?
That’s a valid concern, especially when it comes to stimulant laxatives. These work by essentially irritating the nerves in your colon to force a bowel movement. If you use them too often, your bowel can become sluggish and less responsive, making it hard to go without them. That's why they should only be a short-term fix for acute situations.
On the other hand, osmotic options like magnesium-rich mineral waters are generally much safer for more regular use. They work differently by simply drawing more water into the colon to soften things up.
The goal is always to have your daily habits—diet, hydration, and movement—do the heavy lifting. Think of supplements and other aids as supportive tools, not the foundation of your strategy.
Is It Normal for Constipation to Get Worse with Age?
Yes, it's pretty common for bowel habits to shift as we get older. A few things are usually at play here:
- Decreased Mobility: A more sedentary lifestyle can really slow down a sluggish gut.
- Medication Side Effects: Many common prescriptions for older adults unfortunately list constipation as a side effect.
- Slowing Digestion: As we age, the natural muscle contractions in the digestive tract can simply slow down.
But just because it’s common doesn’t mean you have to accept it. The strategies we've talked about—like focusing on soluble fiber, staying hydrated, and adding gentle movement—become even more critical for staying regular as the years go by.
When Should I Absolutely See a Doctor?
While self-care strategies can be incredibly powerful, they aren't a replacement for professional medical advice, especially if certain symptoms show up. If you've been trying these things for a few weeks without seeing any real improvement, or if you experience any "red flag" symptoms, it's time to check in with a doctor. For a closer look at when complementary therapies might be a good fit, our article on how colonics can help with bloating and constipation has more insight.
It’s definitely time to make a call if you notice any of the following:
- Severe or ongoing abdominal pain
- Blood in your stool
- Unexplained weight loss
- A sudden and lasting change in your bowel habits
A doctor can help rule out any underlying conditions and make sure you're on the right track with a treatment plan that's truly best for your specific situation.
At Healing Waters Wellness Center, we believe in getting to the root causes of digestive issues. Our colon hydrotherapy services are designed to gently cleanse and hydrate your colon, giving your body the support it needs on your path to lasting relief. Explore our holistic therapies today.






